EB Skin Disorder: What It Is, Symptoms, and Treatment Options
Epidermolysis Bullosa (EB) is a rare genetic disorder that makes skin extremely fragile, causing blisters, tears, or sores from minor friction. Symptoms often appear at birth, and early recognition and treatment are vital for managing the condition and improving quality of life.
What is EB?
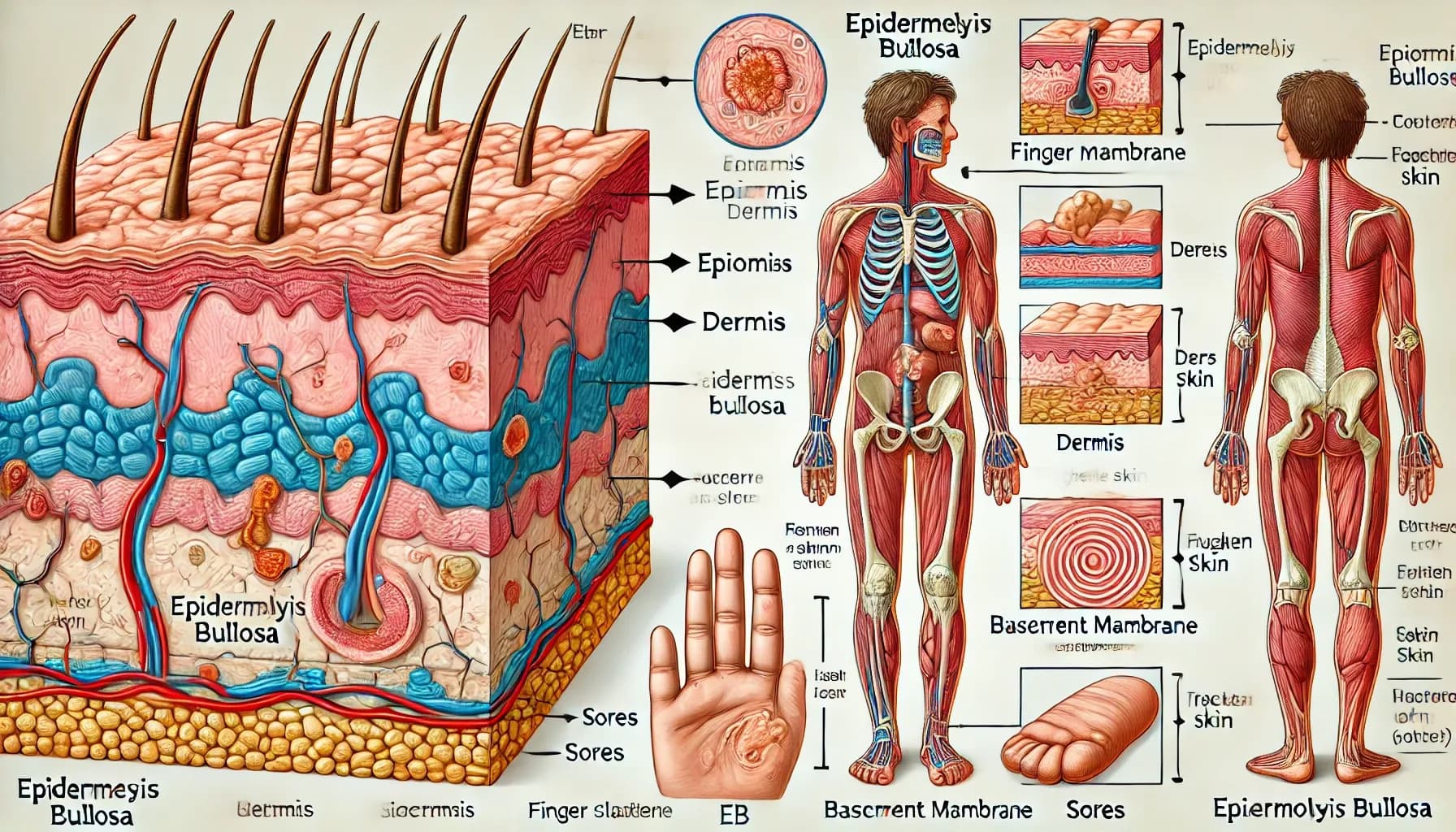
Epidermolysis Bullosa (EB) is a group of genetic disorders that affect the skin’s ability to bind its layers together. In healthy skin, the outer layer (epidermis) and the underlying layer (dermis) are held together by proteins. In people with EB, these proteins are either missing or not functioning correctly, causing the layers to separate easily. This separation results in blistering, open wounds, and increased susceptibility to infection.
There are several types of EB, categorized based on the specific layer of skin affected and the genetic mutations involved. The four primary types include:
- EB Simplex (EBS): Affects the outermost layer of the skin (epidermis). Blisters usually form on the hands, feet, and areas prone to friction.
- Junctional EB (JEB): Affects the layer where the epidermis and dermis meet, often leading to more severe blistering and complications.
- Dystrophic EB (DEB): Affects the dermis and causes scarring and fusion of the fingers and toes in severe cases.
- Kindler Syndrome: A rarer form of EB that affects multiple layers of the skin, leading to a mix of symptoms from the other types.
EB is an inherited condition, and the severity can vary depending on the type and specific genetic mutation involved.
Symptoms of EB
The symptoms of EB can range from mild to severe, depending on the type of EB and the extent of genetic damage. While the most prominent symptom is blistering of the skin, other symptoms may include:
Skin Blisters: Blisters form from minor friction, pressure, or injury. They can occur on the hands, feet, elbows, and knees, but severe forms may affect larger areas.
Open Wounds and Sores: Blisters that rupture can leave behind painful, open sores that are slow to heal.
Thickened Skin on Palms and Soles: Repeated blistering can lead to thickened, calloused skin, particularly on weight-bearing areas like the feet.
Nail Abnormalities: Nails may become thick, misshapen, or completely lost due to repeated trauma.
Scarring and Fusion of Fingers/Toes: Severe cases of dystrophic EB may result in scarring that causes fingers or toes to fuse together.
Dental Issues: People with junctional EB may experience enamel erosion and higher susceptibility to cavities.
Difficulty Eating and Swallowing: Internal blistering in the mouth, esophagus, or digestive tract can cause pain during eating and swallowing.
Increased Risk of Infection: Open wounds provide an entry point for bacteria, increasing the risk of skin infections.
The symptoms can significantly impact daily life, making it challenging to perform regular tasks or participate in physical activities.
How is EB Treated?
While there is currently no cure for Epidermolysis Bullosa, treatment focuses on managing symptoms, preventing infections, and improving the patient's overall quality of life. Treatment strategies often depend on the severity of the condition.
Wound Care and Blister Management
Bandaging and Dressing: Non-adhesive dressings are used to protect wounds and reduce the risk of infection. Specialized dressings are designed to avoid sticking to fragile skin.
Popping Blisters: Large blisters may need to be drained under sterile conditions to prevent them from spreading further.
Moisturizing Creams and Lotions: Keeping the skin hydrated can reduce friction and minimize blister formation.
Infection Prevention and Management
Antibiotic Creams and Ointments: Topical antibiotics are used to prevent infections from open wounds.
Oral Antibiotics: In cases where infections become systemic, oral antibiotics may be prescribed.
Pain Management
Over-the-Counter Pain Relievers: Medications like acetaminophen or ibuprofen can help manage pain from blisters and open sores.
Prescription Pain Medications: For more severe cases, stronger pain relievers may be necessary to manage chronic pain.
Dietary Support
Nutritional Support: People with EB may require a diet rich in protein and essential nutrients to aid in wound healing.
Specialized Feeding Methods: In cases where eating and swallowing are difficult, feeding tubes may be necessary to ensure proper nutrition.
Physical and Occupational Therapy
Mobility Support: Physical therapy can prevent the fusion of fingers and toes and maintain joint mobility.
Assistive Devices: Occupational therapy may provide assistive devices to support daily activities.
Psychological Support
Counseling and Mental Health Services: Coping with EB can be emotionally taxing, especially for children and families. Mental health support can improve emotional well-being.
Emerging Treatments
Gene Therapy: Research is underway to correct the genetic mutations responsible for EB.
Cell Therapy: Scientists are exploring ways to use stem cells to promote skin regeneration.
Protein Replacement Therapy: This therapy aims to introduce missing proteins into the body to improve skin stability.
Living with EB
Managing EB requires a comprehensive approach involving medical professionals, caregivers, and family members. Support groups, educational resources, and access to healthcare professionals can make living with EB more manageable.

