What Is Mycosis Fungoides and What Does It Look Like?
Mycosis Fungoides (MF) is a rare type of non-Hodgkin’s lymphoma that primarily affects the skin. As a form of cutaneous T-cell lymphoma (CTCL), it occurs when cancerous T-cells migrate to the skin, causing a variety of skin-related symptoms. While the exact cause of Mycosis Fungoides remains unclear, it is not contagious and typically progresses slowly over time.
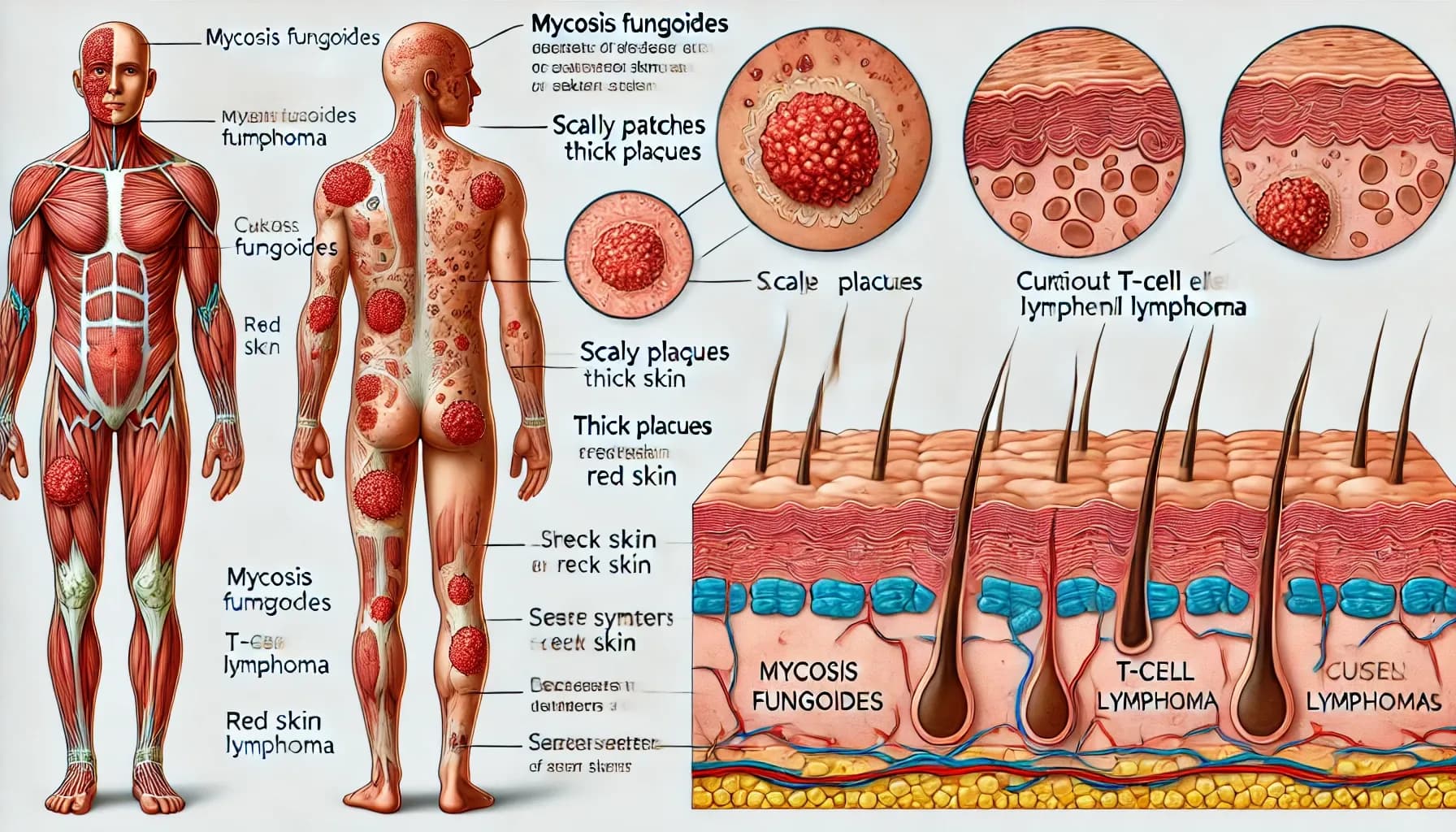
What Does Mycosis Fungoides Look Like?
The appearance of Mycosis Fungoides can vary depending on the stage of the disease. It often mimics other common skin conditions like eczema or psoriasis, making it challenging to diagnose in its early stages. Here’s a breakdown of how it may appear as it progresses:
Patch Stage
- Appearance: Flat, scaly, and discolored patches that may be red, pink, or brown.
- Location: Typically appears on sun-protected areas of the body like the buttocks, thighs, and lower back.
- Texture: Patches may be dry and itchy, resembling eczema or dermatitis.
Plaque Stage
- Appearance: Raised, thickened areas of skin that may be red, purple, or brown.
- Location: May spread to other parts of the body, including the torso, arms, and legs.
- Texture: The plaques often have a rough, scaly surface and are more distinct than patches.
Tumor Stage
- Appearance: Large, raised tumors that protrude from the skin. They may be red, purple, or brown and sometimes ulcerate (develop open sores).
- Location: Tumors can form on any part of the body and may become prone to infection.
- Texture: Tumors may feel soft or firm to the touch, depending on their size and location.
Sezary Syndrome (Advanced Stage)
- Appearance: In this advanced stage, cancerous T-cells spread to the bloodstream. The skin may develop a widespread red, inflamed appearance known as erythroderma.
- Location: Affects large portions of the body, causing intense redness and scaling.
- Texture: The skin may feel dry, itchy, and hot to the touch, similar to severe sunburn.
Symptoms of Mycosis Fungoides
The symptoms of Mycosis Fungoides are primarily skin-related but can change as the disease progresses. Some of the most common symptoms include:
- Itchy Skin (Pruritus): Itchiness is a common symptom, especially in the early patch stage.
- Scaly Patches: Flat, discolored patches of skin that may become itchy and dry.
- Thick Plaques: Raised, hardened areas of skin that feel rough or scaly.
- Tumors or Nodules: Large, raised growths on the skin that can break open or become infected.
- Redness (Erythroderma): Full-body redness, often seen in the advanced stage (Sezary Syndrome).
What Causes Mycosis Fungoides?
The exact cause of Mycosis Fungoides is unknown, but it occurs when T-cells (a type of white blood cell) become cancerous and migrate to the skin. Certain risk factors have been associated with Mycosis Fungoides, including:
Age and Gender: Most common in adults over 50, with men being affected more frequently than women.
Genetic Mutations: Some research suggests that genetic mutations in T-cells may play a role.
Immune System Dysfunction: An impaired immune system may contribute to the development of the disease.
How Is Mycosis Fungoides Diagnosed?
Because Mycosis Fungoides can resemble other skin conditions, it often takes time to receive an accurate diagnosis. Here’s how it’s typically diagnosed:
Skin Biopsy: A small sample of skin is taken and examined under a microscope to detect the presence of cancerous T-cells.
Blood Tests: Blood tests can detect if cancerous cells have entered the bloodstream, which is a sign of advanced disease.
Imaging Tests: Imaging scans like X-rays or CT scans may be used to see if cancer has spread to internal organs.
How Is Mycosis Fungoides Treated?
Treatment depends on the stage of the disease, overall health, and the patient’s response to therapy. Options include:
Topical Treatments
- Corticosteroids: Applied to reduce inflammation and itching.
- Topical Chemotherapy: Drugs like mechlorethamine (nitrogen mustard) may be used to destroy cancer cells in the skin.
- Retinoids: These vitamin A-based creams help slow the growth of cancer cells.
Phototherapy
- PUVA Therapy: Involves using a drug called psoralen combined with UVA light to destroy cancer cells.
- UVB Therapy: Exposes the skin to ultraviolet B light, which can help reduce lesions.
Systemic Treatments (for more advanced stages)
- Oral Retinoids: Retinoid drugs like bexarotene are taken by mouth to slow the growth of cancer cells.
- Chemotherapy: Used when cancer has spread beyond the skin.
- Biologic Therapy (Immunotherapy): Drugs like interferon alpha stimulate the immune system to attack cancer cells.
Radiation Therapy
- Local Radiation: Targets specific tumors on the skin.
- Total Skin Electron Beam Therapy (TSEB): Used to treat the entire body with low-dose radiation.
Stem Cell Transplant
In rare, severe cases, a stem cell transplant may be used to replace damaged bone marrow with healthy donor cells.
Prognosis and Outlook
The prognosis for Mycosis Fungoides depends on the stage at which it’s diagnosed. Early-stage Mycosis Fungoides is treatable, and many people live for decades with proper management. Advanced stages, particularly Sezary Syndrome, are more challenging to treat. Early detection, ongoing care, and access to specialized medical support can significantly improve outcomes.


